Neuroendocrine Tumor Therapy
In this group of tumors are included: carcinoid; gastroenteropancreatic tumors (gastrinoma, insulinoma, vipoma); pheochromocytoma, paraganglioma, neuroblastoma, medullary thyroid carcinoma, lung small cell cancer, etc. The most frequent is the carcinoid tumor which causes the carcinoid syndrome with diarrea, hypotension, facial flushing, etc..
The active uptake of MIBG (Meta-Yodo-Benzyl-Guanidine) a cathecholamine analog, by tumors derived from neural crest and a high tumor retention, have allowed in certain cases, the therapeutic use of 131-I-MIBG. Over 90% of pheochromocytomas and neuroblastomas, about 35% of medullary thyroid carcinomas and 70% of carcinoid tumors concentrate high amounts of MIBG.
Additionally, somatostatin analogs can be employed to treat neuroendocrine tumors, especially carcinoids, due to the fact they have receptors in 80% to 90%, mainly sst type 2. Except insulinoma with 50% to 61%.
These therapies must be considered essentially palliative, unless given at very early disease stage and with small lesions, then can be targeted adequately are more effective and be eventually curative.
Disadvantage comprise effects such as bone marrow suppression, with
platelet and leukocyte cell count diminution. Leading to bleeding and
infections. Likewise, renal function involvement though in small percentage of
cases, especially if protective measures are used such as amino-acid infusion.
Also, retroperitoneal fibrosis. Consider more rarely, irradiation of of the
bowel and eventual complications such as bleeding or rupture. These effects are more pronounced with 90-Y peptides than 177-Lu Dotatate.
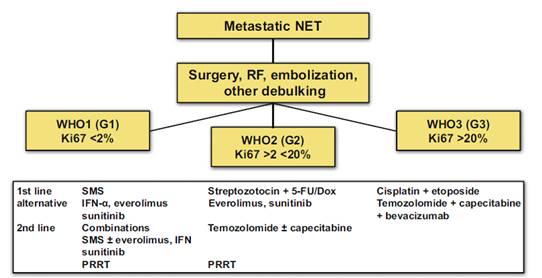
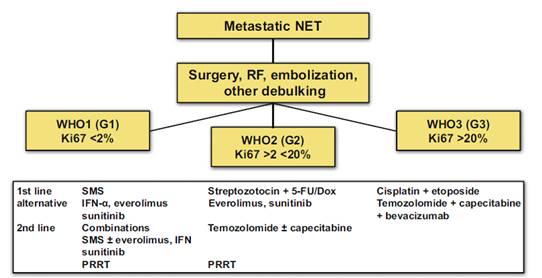
Oberg K.E. comments the algorithm displayed below, to decide which type of therapy to select on patients with neuroendocrine tumors, according to Ki67 marker obtained from the tumor biopsy (1).
SMS=somatostatin analogue octreotide; IFN-α=interferon; PRRT=Systemic peptide receptor-targeted radiotherapy.
Ki-67 is a protein in the cell nucleus during cell division and is a marker of tumour proliferation (grade and prognosis). Patients with low Ki-67 levels (<2% of positive cells) have lower-grade tumours and survive longer.
References:
1 Oberg K.E. The Management of
Neuroendocrine Tumours: Current and Future Medical Therapy Options. Clinical
Oncology 2012; 24: 282-293.
Home Index Clinical Nuclear Medicine Diagnostic Techniques Therapeutic Methods